What Can I Do?
Module 2: What Can I Do?
What does S.A.V.E.S. stand for?

S.A.V.E.S.14 is an acronym for action that identifies the five components of helping someone experiencing suicidal behavior:
- Signs of suicide
- Ask about suicide
- Validate feelings
- Expedite referral
- Set a reminder to follow up
Signs of suicide
 Warning signs are behaviors that indicate someone may be at immediate risk for suicide.15 It is not always easy to recognize when someone is suicidal, but there are some warning signs that you may be more likely to observe in a pharmacy setting. Some people who die by suicide may only exhibit one, others may show several signs, and some may show no signs at all.
Warning signs are behaviors that indicate someone may be at immediate risk for suicide.15 It is not always easy to recognize when someone is suicidal, but there are some warning signs that you may be more likely to observe in a pharmacy setting. Some people who die by suicide may only exhibit one, others may show several signs, and some may show no signs at all.
Person talks about:
|
Person exhibits:
|
|
“The patient said he didn’t know why he was even buying any of the medication because hopefully he wouldn’t be around long enough to take it.”
-Community Pharmacy Technician
|
“We had a patient we absolutely loved. They would come in every time to pick up their medicine with a cheerful attitude. They were always well dressed, and they always would stand around and talk to us for a little bit before leaving. Recently this patient has come in upset, fatigued, and looking disheveled all the time.”
-Community Pharmacy Technician
|
- Threatening to hurt or kill oneself
- Looking for ways to kill oneself (i.e., seeking access to pills, weapons, or other means)
- Exhibiting self-destructive or risk-taking behaviors
Ask about suicide
 In 2019, suicide was a Top 10 cause of death in the U.S. It is time for suicide to become a part of our conversations. If you think that your patient is at risk, asking the question up front is important, even if it is uncomfortable.
In 2019, suicide was a Top 10 cause of death in the U.S. It is time for suicide to become a part of our conversations. If you think that your patient is at risk, asking the question up front is important, even if it is uncomfortable.
Think about it another way. Imagine you are in the patient’s position. How would you feel if you were in crisis or considering suicide, and your pharmacist had not asked? Or ignored the signs?
“Are you thinking about killing yourself?” can be an awkward and uncomfortable question to ask, but it is an effective method to find out if a person needs help. Tips for how to make this potentially life-saving inquiry are provided below.
- Ask the question in a natural way.
- Ask whenever there are warning signs.
- People experiencing a crisis want someone to ask.
- Asking reduces the stigma associated with having suicidal thoughts.
- Don’t ask the question in a way that sounds like you are expecting a “No” answer.
- Example: “You aren’t thinking about killing yourself, are you?”
Other things to consider when talking with a potentially suicidal person:
- Remain calm
- Listen more than you speak
- Be confident
- Do not argue
- Use open body language (maintain eye contact, nod to show attentiveness, uncross your arms)
- Use supportive and encouraging comments
Validate feelings
Validation means that you recognize, acknowledge, and value your patient’s feelings. Engage in active listening, give the patient your full attention, and do the following:
- Acknowledge their feelings
- Listen and allow the person to talk
- Do not judge
- Reassure the person that help is available, and you will help them find it
 “She (the cashier) asked if I would take some time to meet with the patient in our private consultation room, which I agreed to do. She was absolutely broken. She gave me a very detailed history of her experience (on two separate occasions) while on an involuntary hold at a facility. I may have gotten in ten words. But I didn’t need to say more. She didn’t need me to say more.”
“She (the cashier) asked if I would take some time to meet with the patient in our private consultation room, which I agreed to do. She was absolutely broken. She gave me a very detailed history of her experience (on two separate occasions) while on an involuntary hold at a facility. I may have gotten in ten words. But I didn’t need to say more. She didn’t need me to say more.”
Expedite referral
- Connect the individual with services. Even for individuals who deny suicidal behavior, provide them with information for the Crisis Line.
- Encourage the patient to stay in the pharmacy. If you think they may leave before you can connect them to help, try asking them to hold something, like a pen or a pamphlet, to keep them at the counter while you call the Crisis Line.
- If you can’t reach someone immediately on the Crisis Line, please go to the Referral Tool located in the Resources tab for additional national, state, and local resources.
The Veterans Crisis Line is for veterans, servicemembers, and anyone concerned about their well-being. Support is…
- Free
- Confidential
- Available every day, 24/7
Assist the person in finding a care facility by personally referring them, arranging transportation, calling, or providing the appropriate resource(s). Do not leave the person alone. Stay with them until they are safe.
- We have included a resource referral tool on this website. Here you will find national resources, as well as resources by county or zip code readily available for people in crisis. These services include help for mental health crisis, substance use disorders, and veteran specific services.
- Click here to learn what to expect when calling the Crisis Line.
|
Patient exhibits warning signs Ask
“Are you considering suicide?” If No
If No Response
Provide the patient with the Crisis Line number. If Yes
Unsure of immediate danger or passive suicidal behavior: Ask if you can call the Crisis Line for the patient or provide the Crisis Line number. Provide referral resource tool information. Click here for an example. Patient has shared a plan: Call the Crisis Line or encourage the patient to call the Crisis Line. Monitor the patient until they connect with crisis services. Click here for an example. Patient has shared they have taken harmful action: Call 911. If at pharmacy, stay with the patient. If on the phone, try to stay on the line until emergency personnel arrives. Click here for an example. Set a reminder to follow up with the patient the next day. 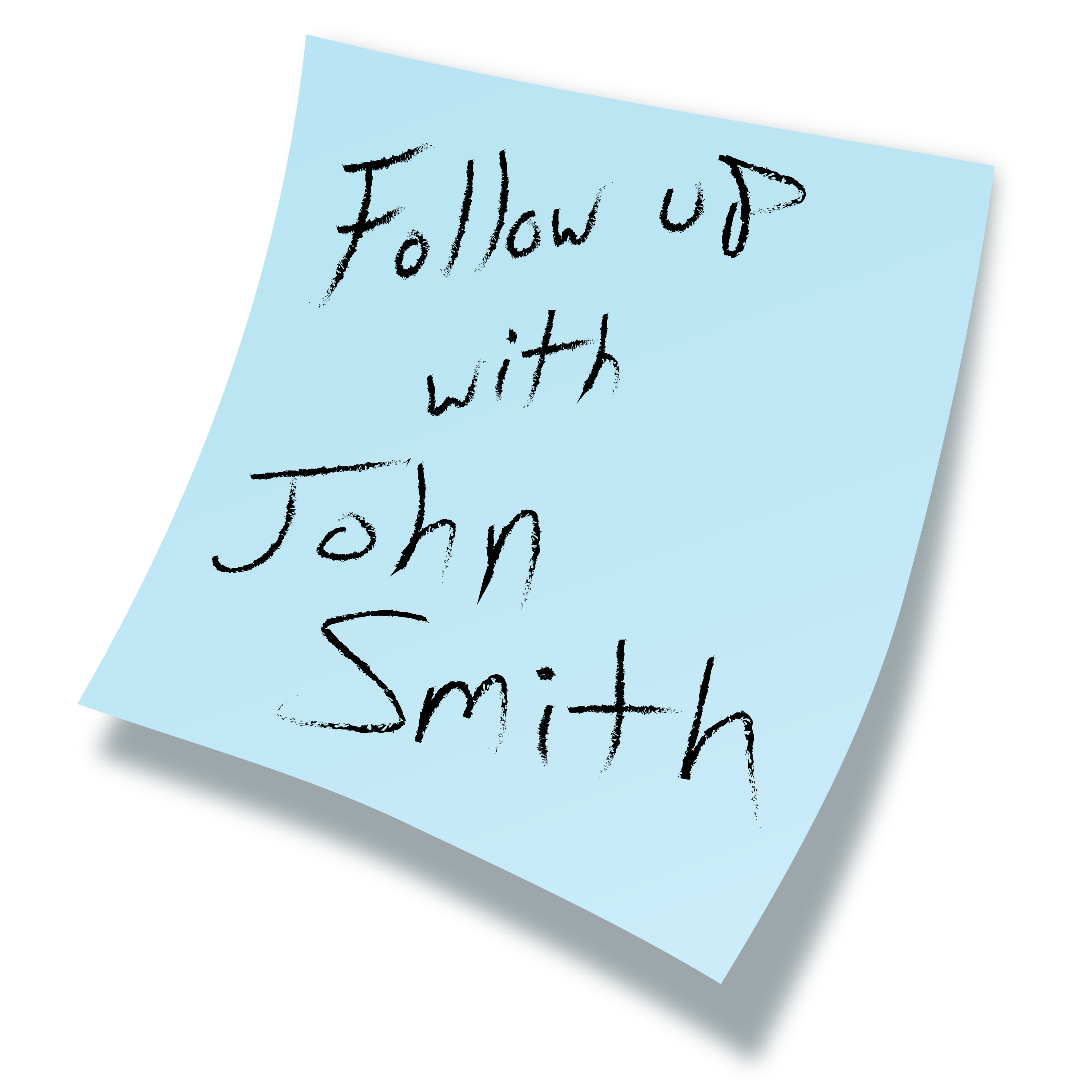 |
Signs
Ask
Validate/empathize
Expedite referral
Set a reminder to follow up
|
Practice responding ahead of time
Try to remain calm
Be direct
Allow the patient to talk
Show that you care
|

- The Veterans Administration (VA) and Department of Defense (DOD) both provide employees who work at the Crisis Line.
- Service members, veterans, and their families or friends who are concerned about them are encouraged to call the Crisis Line and press “1” or text 838255 for immediate crisis resources.
- ANY veteran or service member can be served by option 1, regardless of eligibility for VA benefits.
- An advantage to choosing option 1 is that the VA and DOD staff have access to the same protocols as the main number, in addition to scheduling and other resources only available to veterans and service members.
- The Veterans Administration also has an online chat service that is available 24 hours a day.
Set a reminder to follow up
 Current best practice recommends following up the next day with patients who show suicide warning signs. It’s easy to forget to do this, so it’s important to remind yourself to follow up:
Current best practice recommends following up the next day with patients who show suicide warning signs. It’s easy to forget to do this, so it’s important to remind yourself to follow up:
- Make a note to connect with the person the next day
- Use a method that works within your clinical workflow
The note to follow up could be as simple as leaving a sticky note on your computer or setting a calendar reminder to follow up.
Your follow-up conversation can be short and to-the-point. (See the videos in the “How does it work?” section for examples.) Just let the person know who you are and that you wanted to check in to see if they are okay.